Written by Chowa Tembo Kasengele, MS, BSN, and Ilana R. Siegal, MD, MA from the Stillbirth Advocacy Working Group
According to Zambia’s new Bereavement Training Guidelines, “don’t worry, God will give you another child” is not a reassuring phrase for expectant mothers coping with stillbirth; no parent can know God’s plan, so the promise of a future child does not console the loss of one in the present.
In the Mansa District, over 30 Zambian health workers, including midwives, nurses, obstetricians, general practice doctors, ultrasound technicians, and nursing and midwifery students, were trained in Advanced Bereavement Care (ABC) through the Lugina Africa Midwives Research Network (LAMRN). LAMRN was a network of midwives and stakeholders from six African countries collaborating with The University of Manchester and Liverpool University in the UK. The organization’s mission was to improve midwifery knowledge, practice, and evidence-based research to improve reproductive health in the region.
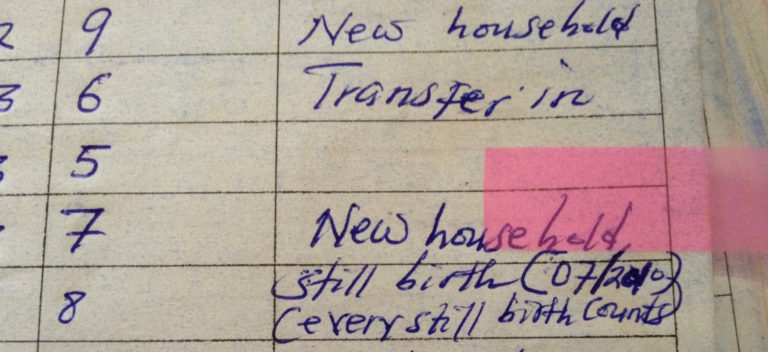
The World Health Organization (WHO) reported Zambia’s stillbirth rate at 14.8 per 1,000 total births in 2019, down from 19.6 in 2004. However, due to cultural, systematic, and geographic factors that contribute to under-reporting of stillbirths, this statistic is most likely an underestimate. Many women give birth at home and stillbirths are socially and statistically invisible. A lack of government-issued stillbirth certificates and no funerals keeps the problem in the dark. Having worked as LAMRN Zambia Project Lead, Chowa Tembo Kasengele (one of the authors) addresses stillbirths in Zambia by developing bereavement support for parents and strengthening stillbirth civil registration. Since LAMRN training was limited to Mansa District health workers, she is currently seeking financial support to scale up ABC training of health workers in the remaining 11 districts in Luapula Province.
Chowa is passionate about exploring the cultural factors that drive stillbirth practices. Without a culturally relevant approach to education about and care after stillbirth, Zambia and other countries face challenges in countering the narratives that maintain the stillbirth taboo and reduce data transparency. As an example, when a Zambian woman has a stillbirth, she should avoid crying to prevent subsequent stillbirths. She must refrain from seeing or touching her stillborn baby, or even following the stillborn baby to the graveyard. Stillborn babies are sometimes put in the sluice room, the “dirtiest room” in the health facility, awaiting disposal. Does this mean a stillborn baby is considered “dirty?” Chowa challenged health workers undergoing ABC training to find a more dignified place for stillborn babies to “rest” before their final “disposal”.
To address maternal isolation and depression after suffering a stillbirth, Chowa works with a network of women in Mansa District called the Public Private Involvement (PPI) group. Women in the PPI group have experienced stillbirth themselves and now comfort and support grieving mothers and families through church platforms, community meetings, radio stations and health facilities. Chowa has witnessed improvements in maternal wellbeing with the initiation of bereavement training for many healthcare professionals. Providing bereavement training creates a safe space for families to process their loss, gives dignity and respect to the deceased baby, and “makes stillbirths count.”
“When I was diagnosed with a stillbirth during labor, the Midwives treated me with respect and explained what was happening. The baby had the umbilical cord around its neck tightly. I felt supported by the Midwives; indeed, things have improved at the hospital.” (Puerperium mother)
‘’Having undergone the ABC training, we have established a stillbirth clinic to help prevent subsequent stillbirths.’’ (Obstetrician, Midwife)
This post from the Stillbirth Advocacy Working Group (SAWG) reflects the perspective of the authors alone; it does not represent the views of the SAWG. The Stillbirth Advocacy Working Group was founded by the Partnership for Maternal, Newborn and Child Health, and is co-chaired by the International Stillbirth Alliance and the London School of Hygiene & Tropical Medicine. Email co-chairs Hannah Blencowe or Susannah Leisher at hannah.blencowe@lshtm.ac.uk or susannah.leisher@hsc.utah.edu.To learn more or sign up to join the group by emailing sawg@stillbirthalliance.org.
 Chowa Tembo Kasengele, MS, BSN is a Zambian Registered Nurse Midwife by profession. She possesses a Master of Science degree in clinical research from the University of Manchester and a Bachelor of Science in nursing from the University of Zambia. She is a qualitative researcher and served as the Principal Investigator and Country Lead on the Stillbirth Prevention and Management Project in Zambia through the Lugina Africa Midwives Research Network (LAMRN) from 2017 to 2021. She is the Chief Nursing Officer for Adolescent Health at the Zambian Ministry of Health Headquarters where she works to improve equality and equity for young people through universal health coverage to leave no one behind. Chowa is a committed member of the SAWG and ISA in the quest to help facilitate reduction of stillbirths through knowledge and practice exchange with other member countries. Chowa is actively pursuing donor support to scale up and sustain ABC training of health providers. Additionally, she is seeking funding to support her doctoral studies which will focus on developing skills to conduct a qualitative analysis of the cultural practices surrounding stillbirths in Zambia.
Chowa Tembo Kasengele, MS, BSN is a Zambian Registered Nurse Midwife by profession. She possesses a Master of Science degree in clinical research from the University of Manchester and a Bachelor of Science in nursing from the University of Zambia. She is a qualitative researcher and served as the Principal Investigator and Country Lead on the Stillbirth Prevention and Management Project in Zambia through the Lugina Africa Midwives Research Network (LAMRN) from 2017 to 2021. She is the Chief Nursing Officer for Adolescent Health at the Zambian Ministry of Health Headquarters where she works to improve equality and equity for young people through universal health coverage to leave no one behind. Chowa is a committed member of the SAWG and ISA in the quest to help facilitate reduction of stillbirths through knowledge and practice exchange with other member countries. Chowa is actively pursuing donor support to scale up and sustain ABC training of health providers. Additionally, she is seeking funding to support her doctoral studies which will focus on developing skills to conduct a qualitative analysis of the cultural practices surrounding stillbirths in Zambia. Ilana R. Siegal, MD, MA is a recent graduate of Wright State University Boonshoft School of Medicine in Ohio. She participated in the Epidemiology Elective Program through the Centers for Disease Control and Prevention (CDC). She interned at the National Center for Health Statistics (NCHS) in the Division for Vital Statistics, Mortality Statistics Branch. She earned her B.A. in international relations at Syracuse University with concentrations in international political economy and the Middle East. She followed with an M.A. in Bioethics at Case Western Reserve University, where she studied women’s and public health practices in The Netherlands. Clinical and social outreach experiences in Nicaragua, Israel, Cuba, and Eswatini inspired Ilana to fight for equitable access to medical care worldwide.
Ilana R. Siegal, MD, MA is a recent graduate of Wright State University Boonshoft School of Medicine in Ohio. She participated in the Epidemiology Elective Program through the Centers for Disease Control and Prevention (CDC). She interned at the National Center for Health Statistics (NCHS) in the Division for Vital Statistics, Mortality Statistics Branch. She earned her B.A. in international relations at Syracuse University with concentrations in international political economy and the Middle East. She followed with an M.A. in Bioethics at Case Western Reserve University, where she studied women’s and public health practices in The Netherlands. Clinical and social outreach experiences in Nicaragua, Israel, Cuba, and Eswatini inspired Ilana to fight for equitable access to medical care worldwide.