Photo caption: Stable, at-risk babies receiving required care including KMC in a room adjacent to the postnatal ward labelled as the “Small Baby Ward” at the Sucheta Kriplani Hospital, Lady Hardinge Medical College, New Delhi, India. (Photo, courtesy, Dr. Sushma Nangia, Director Professor & Head Neonatology, Lady Hardinge Medical College, New Delhi, India)
Over the last two decades newborn health in low- and middle- income countries (LMICs) initially focused on essential newborn care and basic care for all babies at community and facility levels. More recently, with prematurity being recognized as the major predisposing factor to neonatal mortality, global experts have emphasized care of the “small and sick newborn”. Care was organized across health systems in a three-tiered approach; basic or Level I care in the community and smaller centers; additional intermediate or Level II care at district and regional centers; and, tertiary or Level III care at larger hospitals and academic centers.
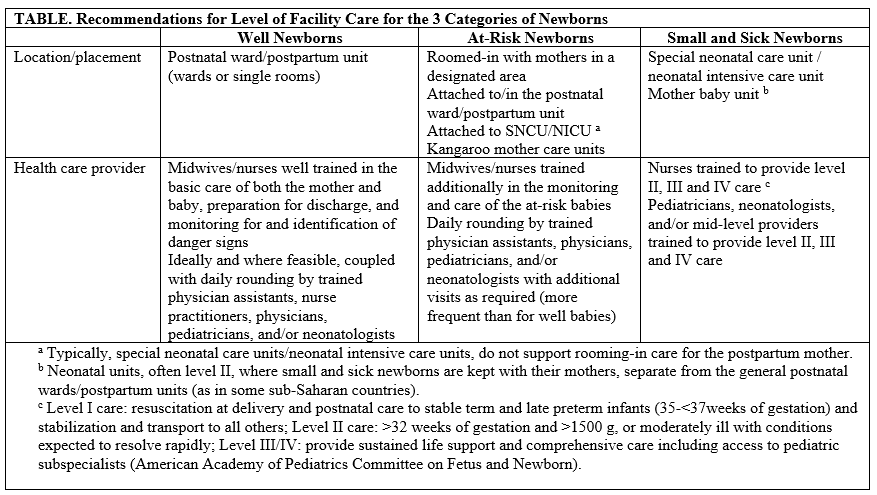
Within individual large hospitals, this translated to well, or healthy, babies staying with their mothers in the postnatal wards, and babies meeting the “small and sick” designation being transferred to Level II special neonatal care units (SNCUs) or Level III neonatal intensive care units (NICUs): a two-tiered approach. In a number of LMICs, while focus on small and sick newborns increased, less attention was directed to care of babies in the postnatal wards. These well infants are often managed primarily by midwives who, based on their training, tend to focus on mothers, providing very basic care for babies. While a number of centers have routine visits by neonatal unit physicians, this is not consistent in all facilities. Thus, to ensure that all babies receive adequate care, babies with predisposing factors for illness are transferred to SNCUs/NICUs, even if clinically stable at birth. While this ensures the safety of this “at-risk” group, it adds to the burden in over-crowded neonatal units that are already short staffed, needlessly separates the mother and baby, and potentially exposes babies to hospital-acquired infections.
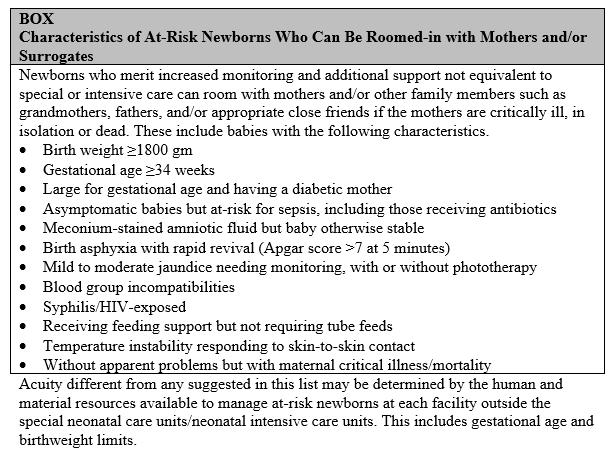
A three-tiered system with an intermediate group of “at-risk” babies will be more advantageous within facilities, instead of the current two-tiered system. These at-risk babies require some additional monitoring to detect any deterioration early, and, at times, some extra care in between that provided in the postnatal ward but not reaching the level of SNCUs/NICUs. This requires some additional training for the postnatal ward staff and counseling of mothers to identify problems as they arise. Such training, however, is much less than the training required for SNCUs/NICU staff. Unless the condition of an at-risk newborn deteriorates and needs more intensive support, the baby can remain with the mother in this intermediate care unit, promoting bonding and exclusive breastfeeding with their inherent advantages.
It is important to realize that this approach is very different to the at-risk approach originally initiated for maternal care in the antenatal period. The original approach focused on providing the necessary care primarily to expectant mothers with risk factors in over-crowded antenatal clinics. We, on the other hand, recommend essential care for all babies, intermediate care for those at-risk newborns, and special (Level II) or advanced intensive (Level III) care for the small and sick babies.
Discussions with colleagues who are currently practicing an at-risk approach have identified locations for this specialized care, in a demarcated area or room adjacent either to the postnatal ward, the neonatal unit, or the pediatric ward. We recommend the postnatal ward option, as both mothers and babies can be cared for appropriately in the early post-partum period. Maternal obstetric care may be challenging if the dyad is moved closer to the neonatal or pediatric unit. Ideally, the demarcated area should be close to the nursing station to allow for quick response. Besides admitting these at-risk babies requiring intermediate care, this area can also be potentially used as a “step-down“ nursery where babies born at the facility who are in SNCU/NICU and have improved and are getting ready for discharge can room with their mothers to promote bonding and breastfeeding and build mothers’ confidence in caring for these recovering infants. Step down nurseries when near the regular neonatal unit can accommodate both inborn and out-born admissions getting ready for discharge with their mothers. Maternal involvement in the care of the baby as a part of family-centered care has been shown to be useful and has not resulted in increased infections.
Examples of the at-risk babies and levels of facility-based care are noted in the below Box and Table.
Separating at-risk newborns into a third category requiring intermediate care within the existing paradigm of the well newborn and the small and sick newborn has the potential to improve the quality of care by right-sizing the level of monitoring and intervention, avoiding needless separation of the dyad, promoting kangaroo-mother care within the framework of family-centered care, and facilitating better prioritized follow-up after discharge.
This approach will require a changed mental model of care and significant advocacy efforts. Policies will need to be reviewed to institute this three-tiered system within hospitals. Ideally, additional midwives will be needed, although some units practicing this approach have managed with existing staff with additional training and rounding by the neonatal unit physicians.
Ultimately, at the regional and national level, it will be essential to carry out advocacy to address the health system and develop suitable policies. While it may initially seem overwhelming, a practical approach would be to have open discussions between Hospital Administration, Departments of Nursing, Pediatrics/Neonatology and Obstetrics and Gynecology to arrive at feasible solutions. In addition, task sharing with the mothers and surrogates will also be a good option to explore where limited human resource issues are a particular challenge. Maintaining necessary data and evaluating the impact will not only help individual facilities to make required adaptations to suit local situations, but also promote expansion to scale.
This blog is derived from the article At-Risk Newborns: Overlooked in Expansion From Essential Newborn Care to Small and Sick Newborn Care in Low- and Middle-Income Countries, published in Global Health: Science and Practice.
