“I became a nurse because my grandmother was a nurse, my sisters are nurses, and one of my aunts is a nurse,” says Neema Kitima, Head Midwife at Bahira Hospital in Bukavu, Democratic Republic of the Congo (DRC). While 80% of births in DRC occur at health facilities with a trained assistant, maternal and neonatal mortality rates remain among the highest in the world. The most recent Demographic and Health Survey (2013–2014) showed that maternal deaths account for 35% of all deaths of women 15–49 years old. Infant mortality is estimated at 28 deaths per 1,000 live births and higher still in rural areas where the newborn mortality rate is 31 per 1,000 live births.
Analyses lead by the Ministry of Health (MOH) have highlighted a number of bottlenecks in service provision across many areas of the health system, including stock-outs, weak referral systems for mothers in need of advanced care, and a low level of training among health care workers. Additionally, poor-quality obstetric and newborn care was identified as major obstacles to improving maternal and newborn survival.

To help the Government of DRC increase mother and child survival, the USAID-funded Integrated Health Project Plus (IHPplus) supported two critical activities: implementing approaches to better integrate maternal and neonatal health care and strengthening information systems to improve the quality of those services. IHPplus was implemented in DRC from June 2015 to June 2018 and was designed to create better conditions for and increase the availability and use of high-impact health services, products, and practices for more than 31 million people in 9 provinces.
Helping mothers survive and helping babies breathe
In response to the different obstacles found by the MOH, the government introduced trainings that integrate interventions, such as family planning, essential obstetric and emergency care, and essential and emergency newborn care. However, the complexity of this training and the absence of trained health care providers limited their impact.
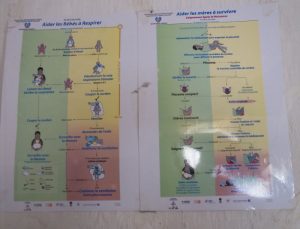
To overcome these challenges, IHPplus coupled the implementation of two approaches, helping mothers survive (HMS) and helping babies breathe (HBB), as innovative strategies to manage postpartum hemorrhage and neonatal asphyxia, both leading causes of maternal and newborn mortality in the DRC.
Health care providers working in maternity wards were trained in the HMS approach. This training included how to prevent, detect, and manage postpartum hemorrhage. Training staff in the HBB approach included skills for essential newborn care, identifying a newborn with asphyxia, and placing them in neonatal intensive care on ventilation by Ambu bag. Mannequins were used to develop these skills.

Neema Kitima received this training while head midwife at Bahira hospital. Thanks to HBB, she says, “we have a clear plan to resuscitate babies who are not breathing at birth, and it works. On average, I use HBB techniques on 2 babies each month out of about 70 women who deliver. One mother I was able to help was a woman whose first-born baby was not breathing. We used the three steps of HBB on him — aspiration, stimulation, and ventilation–before he began to breathe. It was scary for her when she saw her baby not breathing, but because of our training, I knew what to do!”

Results show that globally, HMS and HBB trainings improve providers’ skills in good practices of midwifery, active management of the third phase of pregnancy, and neonatal intensive care. During IHPplus’ three years of implementation, 16,462 newborns with asphyxia were saved using the HBB approach, a success rate of 85%.
Strengthening information systems to improve quality of care for mothers and newborns
The HMS and HBB approaches were only one aspect of IHPplus’ work on maternal and newborn health. Acknowledging that strengthening information systems to support health data is critical, IHPplus, the MOH, and the School of Public Health of the University of Kinshasa did a study to evaluate the availability, quality, and utility of selected indicators (table below) for assessing the quality of maternal and newborn health care in health facilities. The aim of this study was to understand how essential maternal and newborn health data is used in health facilities and how to help health facilities better monitor and improve quality of care for mothers and newborns.
The results of the study showed some inconsistencies regarding the availability of data to make critical decisions. For example, some women are referred without documents, such as an antenatal consultation card, when they arrive to give birth. Other issues regarding the consistency, completeness, and availability of data collection tools were also noted, for example, frequent stock-outs of forms and registers, poor capacity and availability of personnel, and lack of protocols for data analysis.


Considering these findings, the MOH, with support from IHPplus, revised the tools being used for data collection, making relevant data more available for decision making at different levels of the system. After revision, these tools were reproduced and supplied to all health facilities. To promote the use of this data at the facility level, staff agreed that regular monitoring meetings were needed to promote greater use of data. Through these actions, it was also expected that the quality of data would improve over time, both through better skills for data capture and more routine use of collected data.
This blog post is cross-posted from Medium.
View the French translation here.
