In 2017 WHO, Save the Children, UNICEF, and USAID, in collaboration with program managers and policy makers, developed a set of 23 benchmarks to monitor national-level progress in implementation of a new guideline for possible serious bacterial infection (PSBI) in young infants when referral is not feasible. These 23 benchmarks, outlined in the operational guide, were identified covering policy and national coordination, human resources, supply chain management, service delivery and referral, communication and social mobilization, supervision and quality assurance, monitoring, and costing and finance. The benchmarks were designed to help countries assess their readiness to operationalize management of this new guideline and to track progress and scale up as they looked at critical elements for planning and implementation. The benchmarks create a platform for researchers, programmers, decision makers within the Ministries of Health, donors, and stakeholders to review progress, identify barriers, and target priorities for action.
Current status of PSBI adaptation and implementation
By the end of 2019, 26 countries introduced PSBI and are at different phases of implementation. The map below shows progress in operationalizing the guideline for management of sick young infants with PSBI when referral is not feasible.
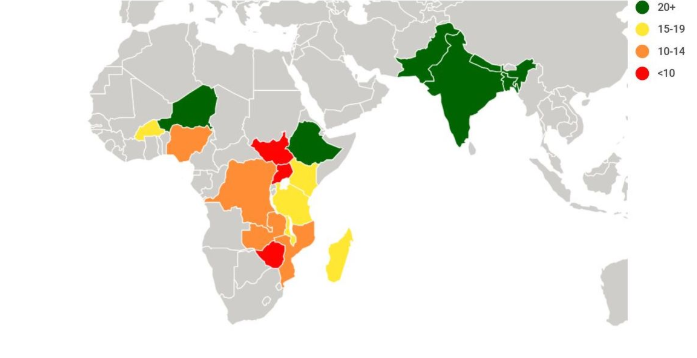
Six countries have fully achieved 20 or more of the benchmarks, five countries have achieved 15-19, four countries achieved 10-14, while three countries achieved less than ten. Countries such as Equatorial Guinea, Burundi, Cameroon, and Liberia have initiated the adaptation process and are preparing for implementation. Myanmar and Indonesia have advanced discussions with policy makers and technical experts on how best to introduce PSBI as part of their national child health strategies.
The summaries below provide more detailed information on the status of implementation using the benchmarks. Each benchmark is rated as “Yes” (green) to indicate that the Ministry of Health is ready to implement or is implementing simplified PSBI management, “Partial” (yellow) to indicate that significant preparations are underway and may indicate what still needs to be completed, or “No” (red) to indicate that there has been little or no progress on this aspect of preparations.
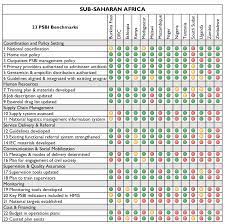
Most countries have coordination mechanisms in place and almost all have adapted their national child health and integrated management of childhood illness (IMCI) guidelines to include management of PSBI where referral is not feasible. It is encouraging to note the number of countries integrating this evidence-based global guideline into national child health strategies and treatment standards. The benchmarks that have faced the greatest challenges are related to communication and social mobilization including engagement of civil society in planning and implementation of PSBI, update of national logistic management and information systems, and costing and financing. Progress among countries is uneven so there is a need for countries to learn from each other. The Health Research Program and CIRCLE Project created the PSBI Community of Practice (CoP) to facilitate learning and sharing of best practices. We strongly encourage everyone to join the PSBI CoP.
Why the benchmarks are helpful
The benchmarks provide priorities for action for decision makers, donors, and development partners working hand in hand with ministries of health. Joint actions are needed for accelerating progress and for addressing implementation challenges. Although the benchmarks have given us a global picture of PSBI implementation at the national level, we should also track progress at the sub-national level. Scaling up PSBI management as part of the overall newborn and child health strategy is critical for achieving Sustainable Development Goals including ending preventable infant deaths.