Integrating postpartum family planning services and counseling into childbirth care is vital to newborn and maternal health and survival.
Offering contraceptive counselling and a wide range of modern methods along the continuum of childbirth care has shown to increase contraception use, which enables women to choose when and if to have a baby. Family planning use is considered postpartum if the woman initiates and uses a method in the first twelve months after childbirth. Postpartum reproductive health and family planning also includes services initiated after miscarriage or abortion. Pregnancies that are spaced by at least two years after a live birth and six months after a miscarriage or induced abortion can reduce the risk of complications and adverse newborn outcomes. Maternal survival is also impacted as women who practice healthy timing and spacing of pregnancies are less likely to die in childbirth or from pregnancy complications. Integrating contraception counseling and services into quality antenatal, postnatal, and newborn care is a proven intervention and should be included in both facility and community based services.
163m
number of women with unmet need for modern contraception services in 2019
1.7m
number of fewer newborn deaths annually if unmet contraceptive need is met in LMICs
700k
number of stillbirths that could be averted annually if unmet contraceptive need is met in LMICS
All data on this page represents the most recent data available, unless otherwise noted. Please visit our Newborn Numbers page and download the Excel spreadsheet to explore the data further.
More on Family Planning
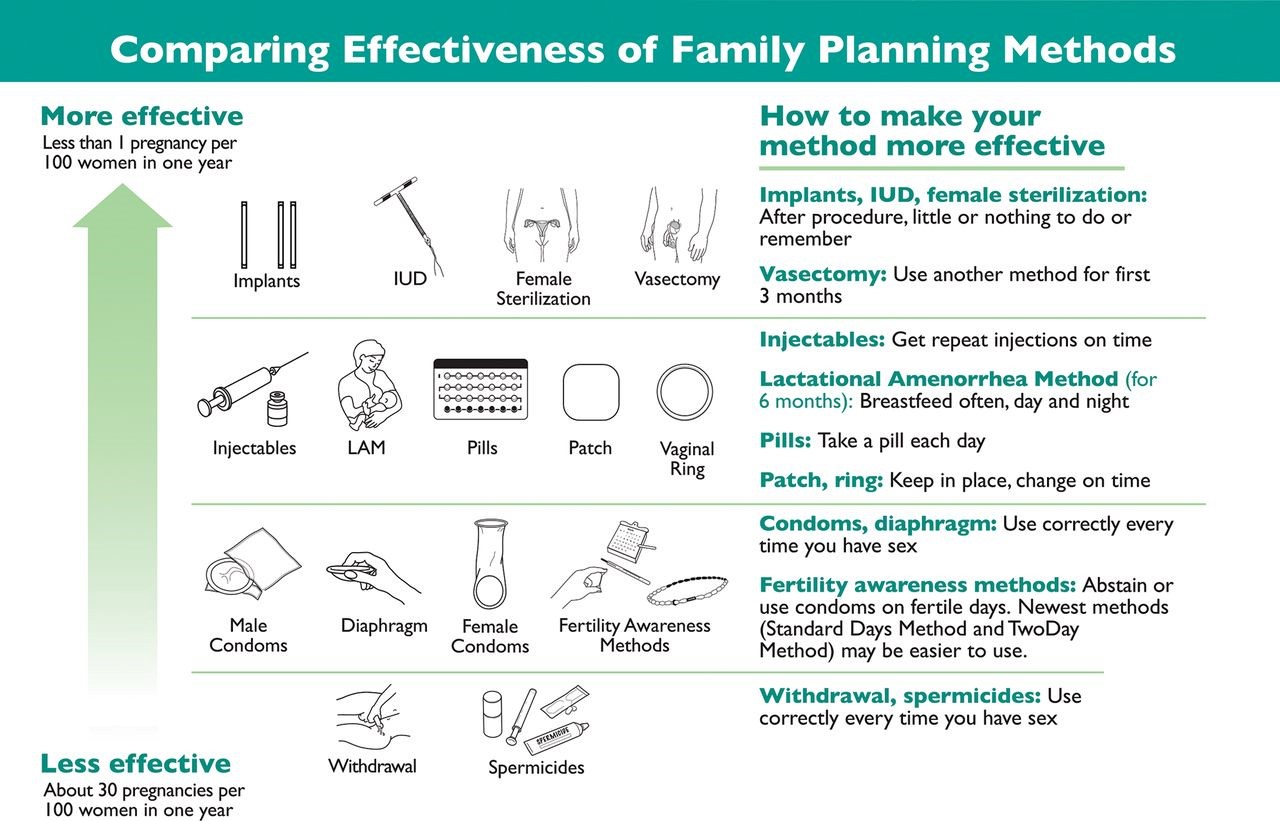
Family planning methods: There are many methods available, under many different brand names. Modern methods include oral contraception pills, implants, injectable, intrauterine devices (IUDs), emergency contraception, male and female condoms, male and female sterilization, and lactational amenorrhea method (LAM). Additional methods include withdrawal, the calendar or rhythm method, and other fertility based methods. Some are more effective than others, and many rely on proper use to ensure effectiveness. Most of these contraceptives can be safely used immediately postpartum; the rest can be initiated shortly after delivery, within a few weeks to six months.
The lactational amenorrhea method (LAM) is 98% effective for the first six months postpartum. LAM prevents pregnancy while the mother is exclusively breastfeeding. It becomes less effective when other foods and liquids, like formula, are included, so women who are unable to exclusively breastfeed should consider other methods.
Spacing of pregnancy: Use of family planning helps achieve healthy spacing of pregnancies, which is critical to a healthy pregnancy and delivery and to newborn survival. When pregnancies are too close together (less than 24 months between the last live birth and the next pregnancy), the risk of low birth weight, preterm birth, and newborn death increases; when pregnancy begins within six months of the last live birth, these complications are even more likely. Furthermore, when a mother who is still nursing an infant of any age becomes pregnant again, it is difficult to meet the nutritional needs of the mother, nursing baby, and fetus.
Timing of pregnancy: Studies have shown that both newborns and mothers have the healthiest outcomes when pregnancies occur after age 18. When mothers are younger than 18, they and their infants face increased risk of birth complications, including stillbirth, low birth weight, and preterm birth. When possible, it is recommended to time pregnancies appropriately, especially by delaying first pregnancy until at least age 18. Adolescents, regardless of marital status, should have access to contraceptive methods to delay pregnancy.
Key resources
- Training Resource Package for Family Planning
- Family Planning Global Handbook for Providers
- High Impact Practices for Family Planning – Immediate Postpartum Family Planning
- Negative effects of short birth interval on child mortality in low and middle income countries: a systematic review and meta analysis
- WHO Family planning/contraception methods
- Postpartum contraception: the lactational amenorrhea method