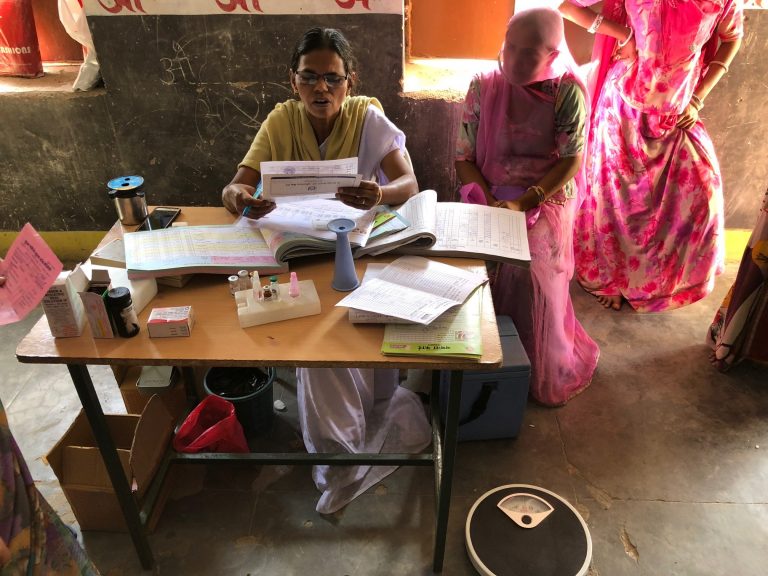
On the surface, health records with completed rows of four antenatal care (ANC) visits for each woman, show great success.
Indicators on antenatal care coverage – at least one visit and at least four visits – focused efforts to achieve the Millennium Development Goals on increasing the number of ANC visits that each woman receives.
However, similar to increases in facility births, these higher numbers did not deliver the expected results in maternal and neonatal survival.
While higher rates of ANC coverage are an important step in improving maternal and neonatal health, they do not tell us about the content of that care. Without assessing and improving the quality of ANC received by all women, we will continue to fall short of our goals to decrease maternal and neonatal morbidity and mortality.
Our recent paper in BMJ Global Health, “Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries,” uses Demographic and Health Survey data from 10 countries to look not only at the number and timing of ANC visits but also the content of those visits. This presented for the first time, a big picture view of the quality of ANC in low and middle-income countries (LMICs).
Using 10 countries as an illustrative analysis, we described ANC coverage (number of visits and timing of first visit) and operationalized indicators for content of care as available in population surveys (reported by women themselves), then examined how these two approaches are related.
10 selected countries: Democratic Republic of Congo (DRC), Nigeria, Rwanda, Zambia, Jordan, Egypt, Nepal, Indonesia, Haiti, and Colombia.

Content of care was assessed using six components routinely measured across all countries, and additional country-specific components (ranging from one to eight per country).
Six routine components:
• Blood pressure measured
• Urine sample taken
• Blood sample taken
• Tetanus protection
• Iron supplementation
• Receipt of information on potential complications
We estimated the percentage of women in need of ANC, and using ANC, who received each component, the six routine components and all components.
The good news was that in all 10 countries, the majority of women in need of ANC reported receiving 1+ ANC visits and over two-fifths reported 4+ visits. However, the receipt of the six routine components varied widely; blood pressure measurement was the most commonly reported component, and urine test and information on complications the least.
Among women who received ANC according to the pattern recommended by WHO at the time (started ANC in the first trimester of pregnancy and received 4+ visits), the percentage receiving all six routinely measured ANC components was low, ranging from 10% (Jordan) to around 50% in Nigeria, Nepal, Colombia and Haiti.
Our findings suggest that even among women with patterns of care that complied with global recommendations, the content of care was poor.
The message is clear: in order to deepen our understanding and monitoring of ANC quality globally, we need to understand far more about the factors promoting and hindering the quality of this care.
The 2016 Lancet Maternal Health Series highlighted the importance of good quality care for every woman, every newborn, everywhere. In a major shift from the 2006 Lancet Maternal Survival Series, attention turned from mortality to morbidity, and the provision of high-quality, woman-centred care was acknowledged as a right.
In late 2016, the WHO released a comprehensive guideline on routine ANC for pregnant women and adolescent girls, adopting for the first time a human rights based approach focusing on person-centred care and wellbeing. This represents yet another important shift towards recognising, and reinforcing, quality of care.
In October 2018, The Lancet Global Health Commission on High Quality Health Systems in the SDG Era (HQSS Commission) will launch its report, offering policy recommendations on care quality at global and national levels in LMICs.
Maternal and perinatal morbidity and mortality remain high: in 2015, an estimated 303,000 women died from pregnancy-related causes, 2.6 million babies were stillborn (half in the third trimester) and 2.7 million newborns died in the first month of life. Good quality maternal health care, including ANC, can prevent the majority of adverse maternal and perinatal outcomes.
In order to achieve the necessary improvements in quality, we must begin to measure and monitor the content of ANC. Efficient and effective action to improve care quality relies on the development of suitable content of care indicators.