ENAP measurement improvement roadmap
The Every Newborn Action Plan (ENAP), is underwritten by a 2014 World Health Assembly Resolution, and aims to support countries in reaching the target of fewer than 12 newborn deaths per 1000 live births, and fewer than 12 stillbirths per 1,000 total births by 2030 [1]. This work is also closely linked to the Ending Preventable Maternal Mortality plan (EPMM), The Global Strategy for Women, Children and Adolescents, and supports the Sustainable Development Goals [2, 3].
Data are crucial to track progress towards this ENAP vision for quality of care at birth. However, there is a major gap for data to track programmatic coverage, quality and service readiness. As seen from programmes such as immunisation, malaria and HIV, these data are fundamental for local programme planning and financing, especially to ensure we reach the poorest families, as well as for global governance [4].
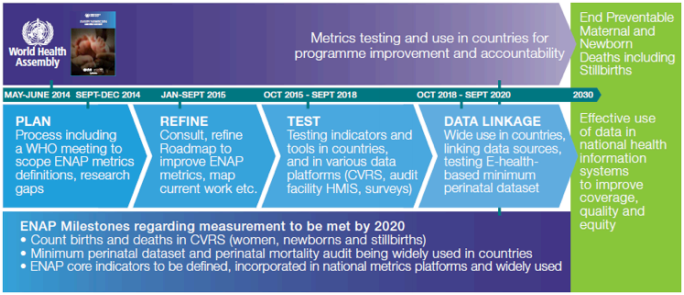
The ENAP measurement improvement roadmap is an ambitious five-year plan to improve, institutionalise and use ENAP metrics in programmes by the year 2020, in order to drive the reduction of neonatal mortality and stillbirths towards 2030 targets. This roadmap, developed through wide consultation, is coordinated via the ENAP metrics group* in combination with EPMM metrics work. Priority indicators between the two strategies have been identified and now there is an urgent need to test and improve programmatic data, especially for coverage of high-impact interventions.
This involves:
- Development of measurement tools, including a focus on strengthening routine health information systems, linking to CRVS and population based surveys
- An ambitious plan to test validity of ENAP coverage indicators in selected facility settings and feasibility of incuding in facility based HMIS
- Intentional transfer of leadership for measurement with links to existing networks for testing, validation, and institutionalisation of the proposed indicators
2.6m
babies are stillborn
(die in last 3 months of pregnancy or during childbirth)
2.7m
newborns die within the first 28 days of life
303,000
women die of maternal causes
Co-chaired by World Health Organization (WHO) and the London School of Hygiene & Tropical Medicine (LSHTM), the ENAP metrics working group has a mandate to work with countries and all partners involved with ENAP to ensure the milestones in the Action Plan related to metrics are met on time, and tools and learning are shared and available in open access for widespread use in countries.
To contact the ENAP Metrics Working Group, please email: enapmetrics@lshtm.ac.uk

ENAP metrics coordination group
The ENAP metrics coordination group includes the following organisations:
Key ENAP metrics activities
The ENAP metrics work stream coordinates the following activities for improving the measurement of corresponding indicators:
- Facility-based metrics testing, especially coverage data, birth weight and birth certificates
- Population-based metrics, especially neonatal mortality rate, stillbirth rate and cause of death
- Service readiness metrics focusing on the inpatient care of small and sick newborns
- Perinatal audit & minimal perinatal data set
- At risk follow up/beyond survival metrics
For additional resources, see ENAP Metrics Resources page
Overall ENAP metrics timeline
Facility-based testing of 1 core EPMM and 4 core ENAP coverage indicators
The first step on the measurement improvement roadmap requires facility-based testing of proposed numerators and denominators for capturing coverage of selected interventions for ENAP and EPMM. The selected interventions include:
- Antenatal corticiosteroids
- Uterotonics
- Neonatal resuscitation
- Kangaroo mother care
- Neonatal infection
- Chlorhexidine cord care
Research overview
The overall aim of this work is to assess the validity of routine health facility-level registers and reporting documentation to measure selected coverage indicators in order to inform use (or not) of these indicators in national and global reporting. In this study, we are aiming to assess to what extent registers or reporting documentation can be used to reliably extract data that can then be used for tallying at that level and in the routine HMIS.
Measurable indicators will later be tested for feasibility at scale, including for the tracking of subnational and national programmes. In addition, this research provides an opportunity to examine a few key metrics to assess coverage, content, quality or safety of these interventions.
This research focuses on the following 5 objectives:
- To test the validity of measuring selected coverage numerators (four for ENAP plus one for EPMM) in routine facility-level registers within a specific health facility, and the validity of the reporting documentation compared to observed data, in order to inform use in routine HMIS
- To analyse a variety of denominator options for use with each numerator
- To examine priority questions with respect to effective coverage (meaning coverage with high quality of care and correct content of care, not just contact)
- To test maternal recall of the practice at discharge from the health facility, as per the first step to assess whether the indicator could be collected during exit interviews in health facility surveys and possibly in household survey
- To assess reported barriers and facilitators to the completion of documentation (such as registers) by health workers.
ENAP metrics facility-based advisory groups
There are five intervention specific advisory groups for the facility-based research.
Country teams and study sites
Bangladesh: International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR, B)
Nepal: UNICEF Nepal
Research data collection tools and timeline
- Labour ward observer checklist
- KMC ward observer checklist
- Neonatal infection data verification tool
- ACS data verification tool
- Maternal recall pre-discharge survey
Funding
Funding from Children’s Investment Fund Foundation (CIFF) is supporting the facility-based testing in Bangladesh and Tanzania, and UNICEF Nepal is supporting the work in Nepal.
Improving the measurement of the ENAP population-based indicators
INDEPTH Network (International Network for Demographic Evaluation of Populations and their Health) is a consortium of Health and Demographic Surveillance System (HDSS) sites in 20 countries, spread over 3 continents. The HDSS sites provide a picture of the health status of the communities through data collection from entire communities over extended time periods (including demographic, socio-economic, environmental, and verbal autopsy) prospectively at least once a year.
The INDEPTH Network’s Maternal and Newborn Working Group (MNWG) main goal is to support coordinated, multi-site generation of evidence to inform policy and programmes for maternal and newborn health and survival in low income countries.
The MNWG of the INDEPTH Network, together with LSHTM, lead on coordinating this research stream to improve population-based metrics around the time of pregnancy and birth, a key priority for the sustainable development goals.

Research overview
The overall aim is to improve the measurement of the ENAP population-based indicators, including birth outcomes, stillbirth and neonatal death, and birthweight and gestational age (GA). Through a competitive process, five INDEPTH network sites were selected to lead on improving measurement of pregnancy outcomes in household surveys.
This research focuses on the following 3 objectives:
- Improve household survey capture of stillbirths and neonatal deaths in terms of assessing pregnancy history compared to live birth history modules
- Improve household survey capture of birth weight and gestational age by assessing various methods for measuring these outcomes in surveys
- Optimise the HDSS data capture of pregnancy outcomes (stillbirths, neonatal deaths, birth weight and gestational age) to link and compare with survey data to examine who is missing and why.
ENAP metrics impact coordination group
The following organisations have key roles in developing this research:
5 INDEPTH HDSS study sites
- Bandim HDSS, Guinea Bissau
- Dabat HDSS, Ethiopia
- Iganga-Mayuge HDSS, Uganda
- Kintampo HDSS, Ghana
- Matlab HDSS, Bangladesh
Research data collection tools and timeline
- Pregnancy history survey
- Birth history survey
- CRVS module
Funding
This research is supported by Children’s Investment Fund Foundation (CIFF).
Improving the measurement of the ENAP input indicators
The first 28 days of life is a vulnerable time for newborns, and direct complications of preterm birth are now the leading cause of child death worldwide. Many lives could be saved, and morbidity prevented, through a combined health systems approach along the continuum of care, with timely provision of quality inpatient care.
In most low and many middle income countries (LMIC), there are very little data available on care for sick newborns, especially on the content and quality of the care that small and sick newborns receive. The data are particularly lacking in settings where access to neonatal special or intensive care is the lowest and where facilities are most in need of targeted efforts to strengthen services and improve the quality of care focusing specifically on the service delivery packages for quality of care of small and sick newborns.
This research stream specifically focuses on improving the measurement of the ENAP input indicators on the service delivery packages for quality of care of small and sick newborns.

Research overview
The overall aim of this research is to improve the data for monitoring service readiness for care of small and sick newborns.
This research focuses on the following 3 specific objectives:
- To carry out a comparative analysis of data from national HMIS with data from the AMDD HFA for select indicators on emergency obstetric and newborn care.
- To carry out a qualitative study with data end users (programme managers, health workers, and ministry officials) to identify barriers and facilitators to improving the data on care of small and sick newborns.
- To provide recommendations to improve the data systems and data collection tools for data on care of small and sick newborns
ENAP metrics service readiness for care of small and sick newborns coordination group
The following organisations have key roles in developing this research:
Malawi study setting
Service readiness data sources
Quantitative data analysis will be carried out using a sub-sample of facilities (mainly focused on hospital level) included in the AMDD EmONC survey and through data available in DHIS2.
The qualitative data collection will be done in the same facilities following completion of the quantitative analysis.
Funding
This research is supported by Children’s Investment Fund Foundation (CIFF).
Despite sustained global progress, rates of stillbirths and neonatal deaths remain high in low resource settings.
Mortality review for stillbirths and neonatal deaths is an important strategy to contribute to global targets and by addressing quality of care at birth and generate data for decision-making.
Perinatal audit is an important part of the ENAP milestones.

Perinatal audit tool
Making Every Baby Count: Audit and review of stillbirths and neonatal deaths
The WHO, in collaboration with ENAP, developed this new international guidance document and accompanying tools to assist countries in their implementation of effective perinatal and neonatal death surveillance and response.
This guide shows the way forward for health-care facilities or whole countries to introduce a system to address the burden of stillbirths and neonatal deaths.
Similar to the maternal death surveillance and response (MDSR) approach to ending preventable maternal mortality, this guide and related tools provide support for identifying cases, collecting information and analysing the data collected to recommend solutions to improve the quality of care and to implement the changes within a continuous evaluation and response cycle.
Pilot countries
- Uganda
- Nigeria
- Bhutan
- Moldova
- South Africa
Timeline
The tools are being piloted in five countries among health workers representing varying types and levels of health facilities.
Results so far show the tools to have excellent acceptability, completeness, ease-of-use, efficacy, and effectiveness in guiding future perinatal death reviews at the health facility level.
This work is ongoing with a series of dissemination webinars planned for early 2017.
To be completed
To contact the ENAP Metrics Working Group, please email: enapmetrics@lshtm.ac.uk

To be completed

